Breast cancer affects up to 1 in 8 women in their lifetime. 20-25% of breast cancers occur in women over 70 years of age. Most screen detected (mammogram and/or ultrasound) cancers have a good prognosis and long term survival for many women.
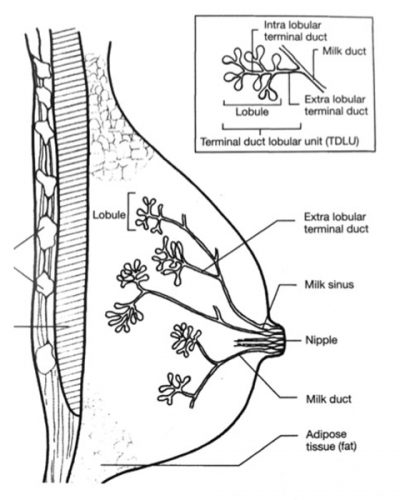
Breast tissue is comprised of lobules (where milk is made) and ducts (pipes that lead out to the nipple).
DCIS (ductal carcinoma in situ) – cancer cells are contained within the duct of the breast and have not invaded the wall of the duct into the surrounding tissue.
Over time, the cancer cells will develop the potential to become invasive breast cancer. Usually a screen detected lesion (via microcalcification or mass) on mammography. Women are usually asymptomatic.
Invasive ductal carcinoma – arises from the ducts of the breast. They are the most common type of breast malignancy.
Invasive lobular carcinoma – arises from the lobular units of the breast. These are more difficult to see on imaging. They can be multifocal.
Arises from the stromal cells of the breast. Can be benign, intermediate/borderline or malignant (very rare).
Patients may present with a symptom (eg. lump, changes in appearance of the nipple or overlying breast skin, discharge from the nipple) or have an area of concern detected on routine breast screening (mammogram +/- ultrasound).
FNA (needle biopsy) or preferably core biopsy is arranged to confirm a diagnosis of cancer. This is usually done under ultrasound or mammographic guidance by a radiologist.
If the results of the needle biopsy or core biopsy are inconclusive, open biopsy (under general anaesthesia) is sometimes needed to obtain a diagnosis.
MRI is occasionally used to better define the extent of disease, and may change surgical management.

Surgery is usually the first step in the treatment pathway for breast cancer.
The goal of surgery is to clear the disease locally and to help guide further treatment (chemotherapy, radiotherapy, hormone therapy).
Breast cancers can be removed by either wide local excision (lumpectomy) – after which the patient is given radiotherapy to the breast or mastectomy, with or without immediate or delayed reconstruction.
The decision as to which procedure is based on the tumour characteristics and the patient.
Invasive cancers require lymph nodes to be removed in order to stage the disease, guide further treatment, control disease locally and give an idea as to prognosis.
In the not so distant past, an axillary lymph node clearance was the treatment offered to most if not all women with invasive breast cancer. This is a procedure associated with considerable morbidity – lymphoedema (up to 40% lifetime risk), restriction in range of shoulder movement and altered sensation in the upper limb. It is now used to manage patients who have lymph nodes involved with cancer.
The concept of the sentinel node has revolutionised management of the axilla. The sentinel node is the first node (or nodes) a tumour will theoretically go to. If this node is removed, and is free from cancer, no further axillary surgery is required and the risk of lymphoedema is reduced to less than 6%.
The sentinel nodes are identified via injection of a radioactive tracer into the breast (injected into the breast before the patient has surgery) and a blue dye (injected into the breast whilst the patient is asleep). The combination of blue and radioactive dye can find the sentinel node in up to 97% of patients.
Not all patients are suitable to have sentinel node biopsy however. Patients who have involved nodes at presentation or who are found to have cancer cells in the sentinel node will need an axillary clearance to manage their disease.
Most patients will only have one operation to manage their breast cancer, however some will require further surgical procedures to treat their disease. This may be in the form of a wider excision around the initial surgical cavity or mastectomy. An axillary clearance is required if the sentinel lymph node contains cancer.
This can be done at the same time as the mastectomy, where skin is spared (skin sparing or subcutaneous mastectomy with immediate reconstruction) or delayed after adjuvant treatments have been completed.
Not all patients are able to have immediate reconstruction, however all patients can discuss their options with a plastic surgeon. Dr Cook can facilitate referral to a plastic surgeon to discuss this and provide the patient with literature about common types of breast reconstruction.
The next steps in the treatment pathway depend upon the pathology results.
Chemotherapy is usually given prior to any other adjuvant treatment. A medical oncologist will plan and supervise this treatment.
All patients who have undergone a wide local excision will be offered radiotherapy after their surgery. A radiation oncologist will manage radiotherapy.
Radiotherapy significantly reduces risk of developing further cancers in the treated breast.
Older patients may be offered a shorter course of radiotherapy.
This is suited to patient with oestrogen receptor positive tumours. Approximately 75 – 80% of breast cancers will respond to the female hormones (oestrogen and progesterone). Patients will be offered medication taken in tablet form daily for 5 years.
Women who have a significant family history of breast malignancy can be offered referral to a clinical geneticist to discuss their risk of carrying a gene associated with an increased risk of developing breast cancer.
Unfortunately breast cancer can affect younger women. Dr Cook can arrange a referral to a fertility specialist to discuss ways to preserve their fertility (including egg retrieval) prior to commencing treatments that may impact upon it (i.e. chemotherapy).
Dr Melinda Cook is a Breast Surgeon consulting at the Breast Health Centre at St Vincent’s Private Hospital Northside, Chermside; Chermside Health Hub; Icon Cancer Centre, North Lakes and the Wesley Private Hospital in Auchenflower.
Dr Cook treats benign and malignant disease of the breast. She participates in the National Breast Cancer Audit and regularly participates in a Multidisciplinary meeting held at the Wesley Private Hospital and St Vincent’s Private Hospital Northside on a fortnightly basis.
Phone: 07 3193 7373
Fax: 07 3319 6727
Postal Address:
PO BOX 206
ASHGROVE QLD 4060
EMAIL: [email protected]